In the fast-paced environment of a hospital, especially a renowned institution like Hartford Hospital, ensuring optimal patient care is paramount. Patient satisfaction hinges not only on medical expertise but also on the quality of their overall experience. Emergency Departments (EDs), by their very nature, are prone to service failures – situations where patient expectations aren’t fully met. These failures, ranging from extended wait times to communication breakdowns, can significantly impact patient satisfaction and even the well-being of healthcare providers. Addressing these lapses effectively through robust service recovery programs, particularly those centered on communication, apology, and resolution, is crucial for institutions like Hartford Hospital striving for excellence in patient-centered care.
The Challenge of Service Failures in Emergency Care
Emergency Departments are inherently complex and unpredictable environments. Daily occurrences can include long waiting times, unexpected testing delays, and, unfortunately, medical errors. These “service failures” are moments where the healthcare experience falls short of patient expectations. For patients already under stress and seeking urgent care, these failures can be particularly distressing, leading to dissatisfaction, anxiety, and a breakdown in trust. Furthermore, unresolved service failures contribute to increased stress and potential burnout among already stretched emergency department staff. Addressing these issues proactively is not just about patient satisfaction scores; it’s about fostering a healing environment and supporting the dedicated professionals who work within it.
Implementing a Proactive Care Program: Communication and Apology as Cornerstones
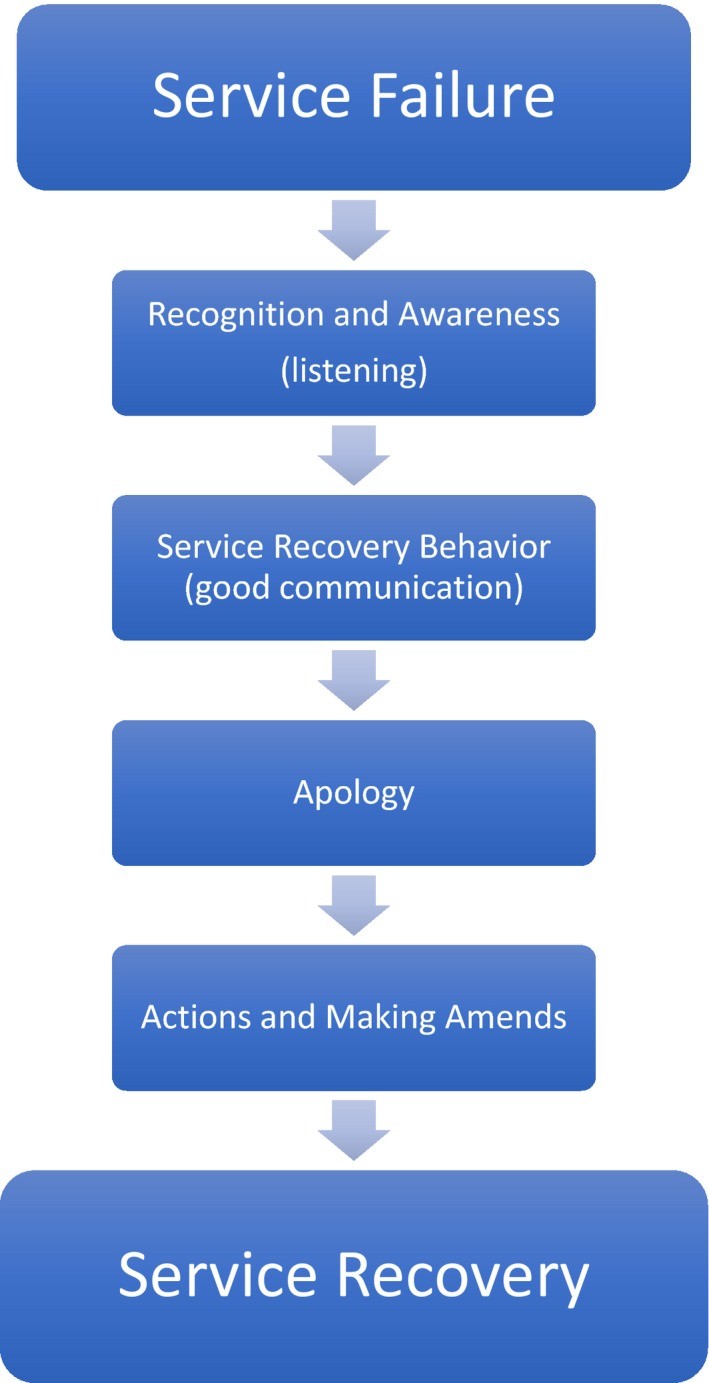
To mitigate the negative impact of service failures, a structured service recovery program is essential. Such a program acts as a framework for healthcare providers to respond effectively when things don’t go as planned. At the heart of any successful service recovery initiative are communication, apology, and resolution. These elements work in concert to acknowledge the patient’s experience, validate their concerns, and actively work towards a satisfactory outcome. Best practices in service recovery emphasize active listening to truly understand the patient’s perspective, delivering a sincere, blameless apology to express empathy without admitting fault, clearly acknowledging the issue at hand, and taking concrete steps to rectify the situation and make amends. Frontline staff, including residents and nurses, are critical in this process as their immediate response significantly shapes the patient’s perception of care and the institution.
Figure 1: Service recovery framework emphasizing key steps for effective patient issue resolution.
Simulation-Based Training: A Practical Approach for Hartford Hospital and Beyond
Recognizing the need for structured training in service recovery, a simulation-based program offers a valuable and practical approach, applicable to institutions like Hartford Hospital and others seeking to enhance their patient care programs. Simulation provides a safe environment for medical residents to practice and refine their communication and service recovery skills without the risks associated with real-patient interactions during the learning phase.
This innovative program utilizes realistic scenarios simulating common service failures encountered in the ED. Postgraduate Year 1 (PGY-1) Emergency Medicine residents participate in these simulations, interacting with trained patient instructors (PIs) who portray patients experiencing service failures. Faculty observers then assess the residents’ communication skills using a modified Master Interview Rating Scale (MIRS) both before and after a targeted service recovery debriefing session. This “pre- and post-intervention” design allows for a measurable evaluation of the program’s effectiveness. The debriefing sessions are crucial, providing residents with evidence-based strategies for service recovery, emphasizing key steps such as recognizing patient dissatisfaction, demonstrating active listening, delivering a sincere apology, and implementing resolution-oriented actions.
Study Findings: Demonstrating Improved Communication and Resolution Skills
The study evaluating this simulation-based program revealed compelling results. While patient instructors, who are extensively trained in using the MIRS, perceived residents’ communication skills as consistently high throughout the program, faculty observers noted a significant improvement in residents’ service recovery communication skills after the debriefing intervention. This difference in evaluation highlights the nuanced impact of the program. Faculty, experienced in assessing resident-level performance, were able to discern a clear positive change in communication skills related to service recovery. This suggests that while baseline communication skills might be present, targeted training is essential to hone specific service recovery techniques. Importantly, resident feedback on the program was overwhelmingly positive, with a vast majority indicating that the training would positively influence their future practice. This subjective endorsement further supports the value and relevance of simulation-based service recovery training in emergency medicine residency programs.
Figure 2: Scatter plots illustrating score variations between rater types pre- and post-intervention, highlighting the impact of the program.
Benefits of a Robust Care Program: Enhancing Patient and Physician Experience
The implementation of a robust service recovery program, incorporating communication and apology resolution training, yields significant benefits for healthcare institutions like Hartford Hospital. For patients, effective service recovery translates to increased satisfaction, greater cooperation with medical advice, and a higher likelihood of returning for future care needs. When service failures are addressed effectively, patients are more likely to have a positive perception of their visit and recommend the institution to others. Furthermore, successful service recovery also benefits healthcare providers. Studies suggest that improved service recovery skills can lead to reduced malpractice risks, decreased work-related stress, and potentially enhanced physician well-being. By equipping residents and frontline staff with the tools to confidently and effectively manage service failures, hospitals can cultivate a more positive and sustainable work environment, alongside improved patient outcomes. Ultimately, investing in care programs that prioritize communication, apology, and resolution is an investment in both patient satisfaction and the long-term well-being of the healthcare team.
Conclusion
This study underscores the effectiveness of simulation-based programs in teaching crucial service recovery communication skills to emergency medicine residents. While consistently high baseline scores from patient instructors suggest a degree of pre-existing communication competence, faculty evaluations clearly demonstrate the program’s success in enhancing specific service recovery skills through targeted training and debriefing. The positive reception from residents further validates the program’s relevance and impact on their perceived preparedness. For institutions like Hartford Hospital, implementing similar care programs focused on communication, apology, and resolution represents a strategic step towards elevating patient care, fostering a more supportive environment for healthcare professionals, and ultimately achieving excellence in patient-centered healthcare delivery. Further exploration and wider adoption of such programs are strongly encouraged to ensure that future generations of emergency medicine physicians are well-equipped to navigate service failures and consistently provide compassionate, effective, and patient-focused care.